Cold Sores (Orofacial Herpes)
Herpes simplex infection of the mouth and face, also known as orofacial herpes simplex, herpes labialis, cold sores, or fever blisters, is a common infection caused by the herpes simplex virus (HSV). Infections with HSV are very contagious and are spread by direct contact with the skin lesions. There are 2 types of HSV: herpes simplex virus type 1 (HSV-1) and herpes simplex virus type 2 (HSV-2). Infections around the mouth, lips, nose, or face are most commonly caused by HSV-1 but can be caused by HSV-2. Both HSV-2 and HSV-1 are common causes of infection of the genitals or buttocks.
HSV causes what is known as a primary infection in most people who are exposed to the virus. Appearing 2-12 days after a person’s first exposure to HSV, the sores of the primary infection last about 1-3 weeks. In the case of orofacial HSV, the sores are usually scattered inside the mouth and are small and painful. These sores will heal completely, but the virus remains in the body, hibernating (latent) in nerve cells.
Certain triggers can cause the hibernating virus to wake up, become active, and travel back to the skin. This is known as recurrent HSV. Recurrent HSV infections may develop frequently (every few weeks), or they may rarely develop. Recurrent infections are milder than primary infections and generally occur in the same general location each outbreak. Recurrent HSV usually appears as a group of blisters (tiny, raised fluid-filled bumps), usually on the lips or around the mouth and nose. These tiny blisters may be preceded by papules (smooth, solid bumps). The papules appear pink or red in lighter skin, and in darker skin, the redness may be more subtle.
Most people get cold sores as children, through contact with a friend or family member who is already infected with HSV. It can be spread (transmitted) by kissing, sharing eating utensils or drinking glasses, or by using personal care items such as the same towel.
Who's At Risk?
HSV infections occur in people of all races / ethnicities, ages, and sexes. Up to 80% of Americans are infected with HSV-1 by the time they are 30.
Signs & Symptoms
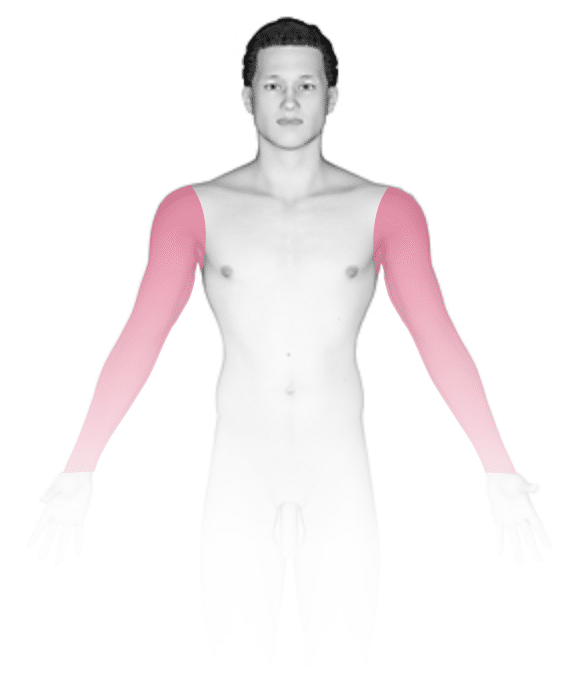
The most common location for primary orofacial HSV infection is inside the mouth. For recurrent HSV, locations include the:
- Lips.
- Nose.
- Chin.
- Cheeks.
There may also be sores inside the mouth, especially if your immune system has been affected, such as by cancer or HIV, or if you have undergone organ transplantation.
In primary HSV, there are painful sores anywhere inside the mouth. The lymph nodes in the neck may or may not be swollen. In severe cases of HSV infection, cold sores may involve the entire lining of the mouth and both lips. These severe infections may be accompanied by fever, sore throat, foul breath, and difficulty eating.
In recurrent HSV infection, there may be one or more tiny blisters that break open and form a scab. Some people experience a warning that blisters are about to appear (called a prodrome), such as tingling or burning of the area. Then, papules appear, followed by blisters.
Additionally, some people never develop the symptoms of a primary HSV infection and may mistake a recurrent infection for a primary infection. A recurrent infection typically lasts 7-10 days. As it fades, it may leave a pink, purplish, or brownish color in lighter skin colors. In darker skin colors, HSV may fade to leave a darker brown color. People who are prone to recurrent outbreaks tend to get them 3-4 times per year.
Triggers of recurrent HSV infections include:
- Fever or illness.
- Sun exposure.
- Hormonal changes, such as those due to menstruation or pregnancy.
- Stress.
- Trauma, such as that caused by dental work or cuts from shaving.
- Surgery.
Self-Care Guidelines
Acetaminophen (Tylenol) and ibuprofen (Advil, Motrin) may help reduce fever, muscle aches, and pain caused by cold sores. Try to drink as many fluids as possible to prevent dehydration. Applying ice packs may relieve some of the swelling and discomfort.
Because HSV is very contagious, it is important to take the following steps to prevent spread (transmission) of the virus during the prodromal phase (burning, tingling, or itching) and active phase (presence of blisters or sores) of HSV infections:
- Avoid sharing cups and eating utensils.
- Avoid kissing and performing oral sex.
- Avoid sharing lip balm and lipstick.
- Avoid sharing razors, towels, and other personal care items.
- Wash your hands with soap and water if you touch an active lesion.
Unfortunately, the virus can still be transmitted even when someone does not have active lesions.
Treatments
Most HSV infections are easy for health professionals to diagnose. On occasion, however, a swab from the infected skin may be sent to a laboratory for viral culture, which takes a few days to grow. Blood tests may also be performed.
Untreated HSV infections will go away on their own, but medications can reduce the symptoms and shorten the duration of outbreaks. There is no cure for HSV infection.
Primary HSV can be treated with oral antiviral medication, such as acyclovir (Zovirax), valacyclovir (Valtrex), or famciclovir (Famvir).
More severe primary HSV infections may require additional medications, for example, a topical anesthetic such as viscous lidocaine, if the areas inside the mouth are very painful. In addition, very severe infections may require intravenous (IV) fluids and even IV antiviral medications or painkillers if the pain prevents you from drinking fluids.
For recurrent HSV, these same oral antiviral medications may help to shorten the outbreak and make it less severe, if taken at the first signs of the outbreak, such as when the prodrome or blisters first appear. People who experience prodromes before recurrent infections may benefit from episodic treatment.
Other people have recurrent infections that are frequent enough or severe enough to justify suppressive therapy, in which medications are taken every day to decrease the frequency and severity of attacks.
Visit Urgency
If you develop tender, painful sores in the mouth or on the lips or nose, see a health professional.
Contact your health professional immediately if an HSV outbreak has not gone away in 2 weeks, if you are avoiding eating or drinking because of the pain, or if you develop blisters or sores near your eye.
If you have an underlying medical condition such as cancer or HIV, or if you have undergone organ transplantation, you are at higher risk for more serious complications. Seek medical advice as soon as possible, especially if you are at risk for more serious complications.
Trusted Links
References
Bolognia J, Schaffer JV, Cerroni L. Dermatology. 4th ed. Philadelphia, PA: Elsevier; 2018.
James WD, Elston D, Treat JR, Rosenbach MA. Andrew’s Diseases of the Skin. 13th ed. Philadelphia, PA: Elsevier; 2019.
Kang S, Amagai M, Bruckner AL, et al. Fitzpatrick’s Dermatology. 9th ed. New York, NY: McGraw-Hill Education; 2019.
Last modified on May 3rd, 2024 at 4:34 pm
Not sure what to look for?
Try our new Rash and Skin Condition Finder













