Eczema (Atopic Dermatitis)
Eczema (atopic dermatitis) is a common, chronic skin condition associated with dry skin that begins with intense itching that is aggravated by scratching and becomes a red, flaky rash. This condition often runs in families and frequently occurs along with other allergic-related conditions such as asthma, hives (urticaria), food allergies, skin sensitivity, and hay fever (allergic rhinitis). Eczema commonly waxes and wanes in response to various environmental factors. Skin infections, excessive heat, winter (or cold, dry climates), fragrances, detergents / soaps, abrasive clothing (eg, scratchy wools), chemicals, smoke, and stress may trigger eczema to flare up or worsen. Scratching increases the chances of developing an infection because it increases breaks in the skin. While these environmental triggers may worsen eczema, they are not the cause of the skin condition.
The primary cause of eczema is an overactive immune system that results in skin inflammation, changes in the normal skin bacteria, and breaks (fissures) in the skin that make individuals more susceptible to bacterial, viral, and fungal infections. The redness, scaling, and thickening of the skin in eczema is a direct result of the increased inflammation in these individuals.
Who's At Risk?
Infants and children are most frequently affected by eczema. Approximately one-third of children with eczema may have disease that persists into their adult years. There is no cure for eczema, and it is not contagious.
Signs & Symptoms
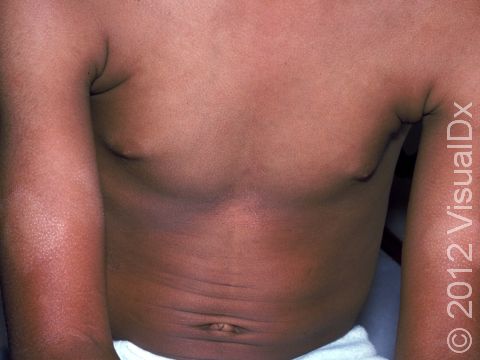
Eczema is usually itchy and presents as a skin rash on the body. The skin lesions are commonly red, scaly, and may appear to be more wrinkled than unaffected skin.
The most common locations for eczema include the skin folds, such as on the face / eyelids, neck, wrists, hands / feet, inner elbows, behind the knees, and genitals. Eczema skin lesions frequently come and go within days to weeks. It is normal for new areas of eczema to appear in various places on the body as others resolve.
Thickened, scaly papules (small, raised bumps) and plaques (areas of raised skin that are larger than a thumbnail and feel rough and flaky) are seen in affected skin areas. The condition may be:
- Localized – A few scattered areas of involvement that are easily treated with self-care measures. Eczema of the hands and/or feet is a common example of localized disease.
- Moderate – More extensive involvement that is more difficult to control with self-care measures and may require topical or other prescription therapy.
- Severe – Widespread involvement that is too difficult to treat with topical prescription therapy and frequently requires the use of more aggressive prescription treatments to keep the skin clear.
Eczema affecting special skin sites, such as the face, scalp, genitals, hands, and feet, may require topical prescription or other aggressive treatments despite a very small amount of skin disease.
In lighter skin colors, affected areas may appear pink or red; however, in darker skin colors, the redness may be subtle or may even appear more purplish or darker brown.
Areas of eczema that become infected with a bacteria, virus, or fungus (known as a superimposed infection) can develop thick yellow-to-orange crusts, blisters, or open skin sores. Secondary skin infections are common in individuals with eczema.
Self-Care Guidelines
Maintaining healthy, moisturized skin is very important for children with eczema.
- Moisturizing daily skin-care routines with fragrance-free moisturizers are essential.
- Avoid long, hot showers or baths. Hot water can dry out the skin, resulting in eczema worsening.
- Hypoallergenic moisturizing soaps, such as unscented Dove, Vanicream bar soap, and Nature by Canus, are recommended.
- Thick moisturizing creams or ointments such as petroleum jelly, Aquaphor ointment, CeraVe healing ointment, CeraVe moisturizing cream, Cetaphil cream, Eucerin cream, and Aveeno cream should be applied to damp skin at least once daily, often after showers or baths.
- Treat red, itchy areas with over-the-counter hydrocortisone cream or ointment 0.5%-1% (eg, Cortaid, Cortisone-10) twice daily. To avoid thinning of the skin, do not use steroid creams for longer than 3 weeks continuously without a 1-week break in between.
- Attempt to minimize exposure to heat, low humidity, detergents / soaps, abrasive clothing, chemicals, smoke, environmental allergens (eg, trees and grasses), and stress.
- Fragrance-free household products and laundry detergent may also be beneficial.
- Keep the home from getting too dry by using a humidifier, especially in the bedroom.
Treatments
Topical or oral (systemic) medications can include:
- Topical steroid creams or ointments to treat active areas of limited (localized) eczema. Low-strength steroids may be used on the face and genitals, and medium-to-high-strength steroids may be used on the body (trunk) and arms or legs (extremities). High-strength topical steroids are frequently required on the hands and feet due to the thickened skin of these body parts. Care should be taken when using topical steroids in skin folds for more than 3 weeks continuously because of the risk of thinning (or atrophy) of the skin.
- Tacrolimus (Protopic) ointment for children 2 years and older, pimecrolimus (Elidel) cream for children 2 years and older, crisaborole (Eucrisa) ointment for children 3 months and older, or ruxolitinib (Opzelura) cream for children 12 years and older may be prescribed in place of topical steroids and are safe on sensitive areas of the body.
- Oral antihistamines may be prescribed to decrease itching or help with associated hay fever.
- A short course of oral steroids may be prescribed for severe eczema, but caution should be taken with oral steroids because severe worsening of eczema can occur when the prescribed steroid course is finished.
- Light therapy (or phototherapy) 3-5 times weekly may be recommended for treatment of widespread or resistant eczema.
- Newer injectable medications known as biologics, such as dupilumab (Dupixent) in children 6 months and older, are the most promising treatments for moderate-to-severe eczema as they are highly effective treatments with very few side effects.
- Janus kinase (JAK) inhibitors, such as upadacitinib (Rinvoq) and abrocitinib (Cibinqo) are oral medications that may be prescribed for patients aged 12 and older with moderate-to-severe atopic dermatitis that is not responsive to other systemic therapies. This class of medication is very effective but should be used with caution given their black box warnings and potential side effects.
- In individuals who have multiple areas of broken skin or a history of bacterial skin infections, diluted bleach baths several times per week may be recommended.
- If an infection is suspected, topical / oral antibiotics, antifungal, or antiviral medications may be prescribed to treat the secondary infection.
Visit Urgency
See your child’s medical professional for evaluation if you notice no improvement with self-care measures or if the condition worsens (flares), or if it involves special skin areas such as the face / eyelids, hands / feet, or genitals.
Also see a medical professional if your child has areas of pus, large numbers of yellow crusty areas, or blisters as these may be signs of a secondary skin infection.
Not all red, scaly rashes on the body are eczema. Many other medical conditions can mimic eczema, such as psoriasis, fungal or other infections, medication reactions, allergic or irritant skin reactions, food allergies or nutritional deficiencies, and other autoimmune conditions. Your medical provider can help you determine the cause of your rash if it is unclear.
Trusted Links
References
Bolognia J, Schaffer JV, Cerroni L. Dermatology. 4th ed. Philadelphia, PA: Elsevier; 2018.
James WD, Elston D, Treat JR, Rosenbach MA. Andrew’s Diseases of the Skin. 13th ed. Philadelphia, PA: Elsevier; 2019.
Kang S, Amagai M, Bruckner AL, et al. Fitzpatrick’s Dermatology. 9th ed. New York, NY: McGraw-Hill Education; 2019.
Paller A, Mancini A. Paller and Mancini: Hurwitz Clinical Pediatric Dermatology. 6th ed. St. Louis, MO: Elsevier; 2022.
Last modified on June 12th, 2024 at 5:19 pm
Related Skin Conditions


Not sure what to look for?
Try our new Rash and Skin Condition Finder