Cutaneous Horn: Diagnosis and Treatment
Cutaneous horn refers to a skin growth that appears as a cone-shaped, horn-like projection caused by overgrowth of the most superficial layer of skin (epidermis). Approximately 40% of cutaneous horns are caused by precancerous lesions called actinic keratoses. Cutaneous horns may also overlie skin cancer (most often squamous cell carcinoma but sometimes basal cell carcinoma), or they may overlie benign growths, such as warts or seborrheic keratoses.
Who's At Risk?
Cutaneous horns most often occur in older adults with lighter skin colors and a history of significant sun exposure. Cutaneous horns can occur in individuals with darker skin colors but are less common. When cutaneous horns occur in children, they usually overlie a wart.
Signs & Symptoms
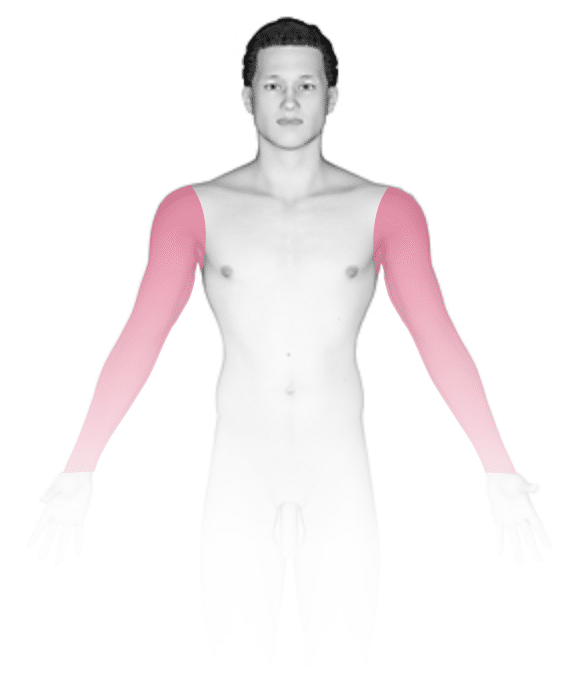
A cutaneous horn most often occurs on sun-exposed areas of the skin and appears as a cone-shaped projection. It has been described as looking like a tiny animal horn. Cutaneous horns are often off-white, skin colored, or darker than the surrounding skin. Cutaneous horns are very hard and can be wide and short or narrow and elongated. Cutaneous horns most commonly appear on the ear, nose, cheeks, backs of the hands, and arms or legs.
Self-Care Guidelines
No self-care is necessary. However, if you have a cutaneous horn, you should see a medical professional so they can determine if the underlying lesion requires medical care.
Treatments
If the lesion the cutaneous horn overlies is benign, no further treatment may be needed.
If the lesion is precancerous, the medical professional may:
- Freeze the lesion with liquid nitrogen.
- Use a topical chemotherapy agent, such as 5-fluorouracil, or a topical medicine that stimulates the immune system, imiquimod.
- Scrape and burn (curettage and electrodesiccation) the lesion.
If the lesion is cancerous, the medical professional may:
- Surgically remove the lesion.
- Use a topical chemotherapy agent, such as 5-fluorouracil, or a topical medicine that stimulates the immune system, imiquimod.
- Scrape and burn (curettage and electrodesiccation) the lesion.
- Recommend radiation therapy.
Visit Urgency
If you have a cutaneous horn or other similar growth on the skin, seek medical evaluation. A biopsy may be needed to assess whether the lesion is benign, precancerous, or cancerous.
Trusted Links
References
Bolognia J, Schaffer JV, Cerroni L. Dermatology. 4th ed. Philadelphia, PA: Elsevier; 2018.
James WD, Elston D, Treat JR, Rosenbach MA. Andrew’s Diseases of the Skin. 13th ed. Philadelphia, PA: Elsevier; 2019.
Kang S, Amagai M, Bruckner AL, et al. Fitzpatrick’s Dermatology. 9th ed. New York, NY: McGraw-Hill Education; 2019.
Last modified on July 25th, 2023 at 1:05 pm
Not sure what to look for?
Try our new Rash and Skin Condition Finder






