Cluster Headache
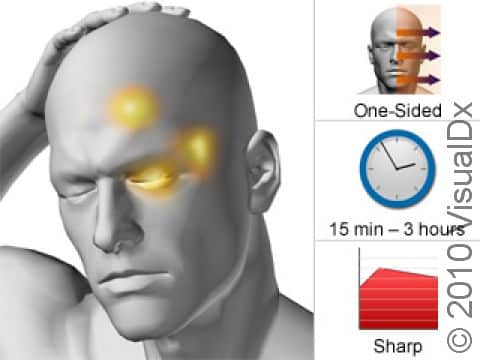
Cluster headaches are recurring severe headaches on one side of the head, typically in or around one eye. These intense headaches cause extreme pain and can wake people from sleep.
Periods of cluster headaches can last from weeks to months, with attacks happening daily and lasting 15 minutes to 3 hours. Cluster headaches can be debilitating, and many people with cluster headaches find it hard to work or continue with their regular daily routines.
Who's At Risk?
Cluster headaches are rare, affecting only about 1% of people. They are more common in men than women. These headaches typically start between ages 20-40 years. Many people who get cluster headaches have a history of smoking or drinking alcohol.
Signs & Symptoms
Cluster headaches involve frequent attacks of severe, short-lasting, one-sided head pain. The pain is usually most intense behind or around an eye, but sometimes the pain occurs in the back of the head. The pain may shift sides between attacks.
Other symptoms of cluster headaches include tearing from the involved eye, red eyes, stuffy nose, and a small pupil and drooping of the eyelid on the affected side. People with cluster headaches may be very sensitive to light and sound.
The pain typically occurs in “clusters,” in which groups of headaches last from 15 minutes to 3 hours. Most cluster headaches last less than an hour. The headaches typically take place 1-3 times a day. Cluster cycles generally last from 2-12 weeks, with most people having 1-2 cluster cycles per year. In people with cluster headache, 10%-20% have the chronic form, which does not occur in cycles / bouts and may have symptoms yearlong.
Cluster cycles can occur at the same time of year for consecutive years, and daily cluster headaches tend to occur at specific times of the day. Headaches are particularly common between 1:00-2:00 AM, 1:00-3:00 PM, and after 9:00 PM. Cluster headaches also commonly occur during the first period of very deep REM sleep, and people will wake with a severe headache 60-90 minutes after going to sleep.
Self-Care Guidelines
Common pain relievers such as ibuprofen and acetaminophen are usually not effective for cluster headaches. Keeping a headache diary, looking for possible triggers for the headache, and trying to reduce stress, such as by trying relaxation techniques, may help improve cluster headaches.
Treatments
For cluster headaches, 3 types of treatments are used:
- Abortive medications to stop a headache that has already started.
- Preventive medications to help reduce the likelihood of headaches during a cluster period.
- Transitional therapy to lessen symptoms until preventive medications are effective.
Inhaled 100% pure oxygen is often used to end a cluster attack, although some people find the headache will start again once the oxygen is stopped. Oxygen can be used numerous times daily for weeks at a time without side effects, though.
Medications called triptans are often prescribed as abortive medications, but these may result in chronic headaches with repetitive use even over short periods of time. Preventive medications should only be used during a cluster cycle and are tapered off when a cluster period seems to be over. Learning about cluster headaches, knowing what to expect, and keeping in touch with your medical professional are key to success in controlling symptoms.
Visit Urgency
All cluster headaches require medical treatment. If you suspect you have cluster headaches, contact your medical professional.
Contact your medical professional if:
- You develop new symptoms not typical of prior headaches.
- You have a particularly severe headache.
- You feel disoriented or lose consciousness.
- Your headache persists longer than 3-4 days (unless this is typical for you).
- Your current treatments or medications are not working.
- Your headache interferes with your daily activities (eg, eating, bathing, working).
Immediately seek medical attention if you or someone you are caring for experiences:
- A stiff neck and a high fever with a headache.
- Loss of motor function (eg, your muscles don’t move normally), inability to think clearly, or convulsions with headache.
- A head injury.
Last modified on October 7th, 2024 at 1:34 pm

Not sure what to look for?
Try our new Rash and Skin Condition Finder