Erythema Toxicum Neonatorum
Erythema toxicum neonatorum, also known as toxic erythema of the newborn, is a harmless rash that appears on the skin of newborns, usually on the second to fourth day of life. This rash goes away on its own and does not cause any pain or itch for the baby. It has often been likened to the appearance of fleabites on the skin. Erythema toxicum neonatorum is extremely common and does not require any treatment as it will go away on its own within hours or days. The cause of this rash is unknown.
Who's At Risk?
Approximately 50% of full-term newborns develop erythema toxicum neonatorum shortly after birth. Preterm infants are less commonly affected; however, they may develop erythema toxicum neonatorum at a week of life. It is also uncommon in infants who weigh less than 5.5 pounds at birth. The rash does not appear to be seen more often in babies of any sex or race / ethnicity.
Signs & Symptoms
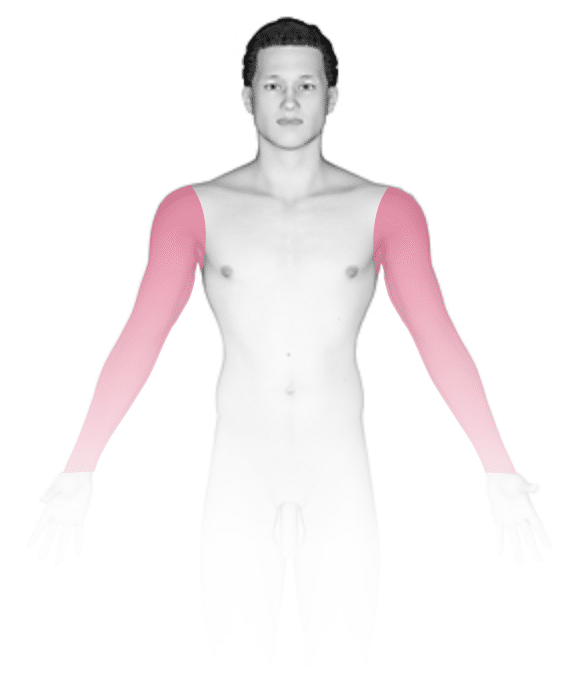
Erythema toxicum neonatorum may initially appear as blotchy, red areas, and then small (1-3 mm), firm, yellow or white pustules (pus-filled bumps) will form on the red areas of skin. In darker skin colors, the redness may be harder to see. There may be just a few or there may be many lesions, and they may be found on any area of the body except the palms and soles. Erythema toxicum neonatorum often begins on the face and spreads, and it may be clustered in areas where there is pressure on the skin. Although it most frequently appears during the first 2-4 days of life, erythema toxicum neonatorum can be seen at birth or may not be present until 10 days of life. New lesions may appear as older ones resolve.
Self-Care Guidelines
There is no self-care for this rash; it will resolve on its own in a few days to a week. Take care to not pop the pustules as irritating the rash may lead to an infection.
Treatments
Your baby’s medical professional will likely not prescribe any medication for this skin condition. If they are not certain about the diagnosis, they may take a sample of pus from the lesions and look at the cells under a microscope. Additionally, a blood test to look for a certain population of cells (called eosinophils) may aid in the diagnosis, although this is not a confirming test and is not commonly done.
Visit Urgency
Because erythema toxicum neonatorum looks similar to many infectious disease rashes, including those caused by the herpes virus or other bacteria or fungi, if your baby has an unexplained rash, consult their medical professional.
Trusted Links
References
Bolognia J, Schaffer JV, Cerroni L. Dermatology. 4th ed. Philadelphia, PA: Elsevier; 2018.
James WD, Elston D, Treat JR, Rosenbach MA. Andrew’s Diseases of the Skin. 13th ed. Philadelphia, PA: Elsevier; 2019.
Kang S, Amagai M, Bruckner AL, et al. Fitzpatrick’s Dermatology. 9th ed. New York, NY: McGraw-Hill Education; 2019.
Paller A, Mancini A. Paller and Mancini: Hurwitz Clinical Pediatric Dermatology. 6th ed. St. Louis, MO: Elsevier; 2022.
Last modified on August 28th, 2023 at 8:39 pm
Not sure what to look for?
Try our new Rash and Skin Condition Finder




